Connect With Us
Blog

Are Heel Spurs Causing Your Heel Pain?
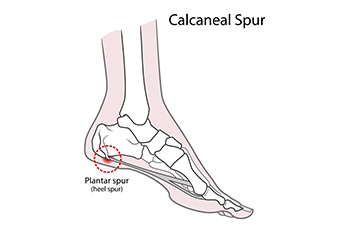
Heel spurs are bony growths that form on the underside of the heel bone, often due to long-term strain on foot muscles and ligaments. They commonly develop along with plantar fasciitis, especially in people who spend a lot of time on their feet, wear unsupportive shoes, or have flat feet or high arches. Symptoms include sharp, stabbing pain in the heel, especially when standing up in the morning or after sitting for a long period of time. While heel spurs themselves may not always cause pain, the inflammation around them often does. The area may feel tender or appear swollen. A podiatrist can diagnose heel spurs with a physical exam and X-rays. Treatment options include stretching exercises, orthotic inserts, anti-inflammatory medications, and cortisone injections. Surgery is rarely needed, but may be considered in severe cases that do not respond to conservative care. If you have ongoing heel pain, it is suggested that you schedule an appointment with a podiatrist who can accurately diagnose and treat heel spurs.
Heel spurs can be incredibly painful and sometimes may make you unable to participate in physical activities. To get medical care for your heel spurs, contact one of our podiatrists from Bangor Podiatry. Our doctors will do everything possible to treat your condition.
Heels Spurs
Heel spurs are formed by calcium deposits on the back of the foot where the heel is. This can also be caused by small fragments of bone breaking off one section of the foot, attaching onto the back of the foot. Heel spurs can also be bone growth on the back of the foot and may grow in the direction of the arch of the foot.
Older individuals usually suffer from heel spurs and pain sometimes intensifies with age. One of the main condition's spurs are related to is plantar fasciitis.
Pain
The pain associated with spurs is often because of weight placed on the feet. When someone is walking, their entire weight is concentrated on the feet. Bone spurs then have the tendency to affect other bones and tissues around the foot. As the pain continues, the feet will become tender and sensitive over time.
Treatments
There are many ways to treat heel spurs. If one is suffering from heel spurs in conjunction with pain, there are several methods for healing. Medication, surgery, and herbal care are some options.
If you have any questions feel free to contact our offices located in Bangor, Gilbert, and Bethlehem, PA . We offer the latest in diagnostic and treatment technology to meet your needs.
How to Treat Heel Spurs
Heel spurs are calcium deposits that cause bone protrusions on the heel bone. Heel spurs are usually associated with plantar fasciitis, which occurs when the plantar fasciitis in the foot becomes inflamed. Typically, heel spurs don’t cause any symptoms. However, they can produce chronic or intermittent heel pain. Those who have had the condition often describe the irritation as a stabbing pain.
There are risk factors that may make you more likely to develop heel spurs. People who have abnormal walking gaits, run and jog on hard surfaces, are obese, or wear poorly fitting shoes are more likely to develop heel spurs.
Fortunately, there are precautions you can take to avoid developing heel spurs. One of the best ways to do this is by wearing well-fitting shoes with shock-absorbent soles. Another preventative technique is to choose running shoes if you plan on running, and walking shoes if you plan on walking. Shoes are made for different activities and it is important to research a shoe before you purchase a pair.
The pain associated with heel spurs often decreases the more you walk. However, a recurrence of pain after an extended period of rest or walking is likely to occur with this condition. Those with severe heel spur pain may opt to go the surgical route for treatment. However, more than 90% of those with the condition get better without surgical treatment. If you have a heel spur and want to know if surgery is right for you, you should go to your podiatrist and he or she will be able to conduct a pre-surgical test or exam to determine if you are an optimal candidate for surgery.
Causes and Risk Factors of a Foot Stress Fracture

A foot stress fracture is a small crack in a bone caused by repetitive force or overuse rather than a single traumatic event. These injuries commonly occur in athletes or individuals who engage in activities with repetitive impact, such as running or dancing. Symptoms often include localized pain that worsens with activity, swelling, tenderness, and sometimes mild bruising. Risk factors include suddenly increasing physical activity, wearing improper footwear, low bone density, and certain medical conditions such as osteoporosis. Stress fractures frequently affect the metatarsal bones in the foot, especially during repetitive motion. If left untreated, these fractures can worsen and lead to more severe injury. If you think you have a foot stress fracture, it is suggested that you promptly contact a podiatrist who can provide an accurate diagnosis and treatment.
Stress fractures occur when there is a tiny crack within a bone. To learn more, contact one of our podiatrists from Bangor Podiatry. Our doctors can provide the care you need to keep you pain free and on your feet.
How Are They Caused?
Stress fractures are the result of repetitive force being placed on the bone. Since the lower leg and feet often carry most of the body’s weight, stress fractures are likely to occur in these areas. If you rush into a new exercise, you are more likely to develop a stress fracture since you are starting too much, too soon. Pain resulting from stress fractures may go unnoticed at first, however it may start to worsen over time.
Risk Factors
- Gender – They are more commonly found in women compared to men.
- Foot Problems – People with unusual arches in their feet are more likely to develop stress fractures.
- Certain Sports – Dancers, gymnasts, tennis players, runners, and basketball players are more likely to develop stress fractures.
- Lack of Nutrients – A lack of vitamin D and calcium may weaken the bones and make you more prone to stress fractures
- Weak Bones – Osteoporosis can weaken the bones therefore resulting in stress fractures
Stress fractures do not always heal properly, so it is important that you seek help from a podiatrist if you suspect you may have one. Ignoring your stress fracture may cause it to worsen, and you may develop chronic pain as well as additional fractures.
If you have any questions, please feel free to contact our offices located in Bangor, Gilbert, and Bethlehem, PA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Stress Fractures of the Foot and Ankle
Our bones are important aspects of our body and they are constantly changing. The heavier the workload for a bone, the more likely it is that calcium will be placed in it. When a bone isn’t used often, there won’t be much calcium within it. When stress from repetitive loads prevent the bone from being able to repair itself, cracks will start to form. Stress fractures are defined as cracks in a bone that result from repetitive force, such as overuse.
The most common cause of stress fractures is a sudden increase in intensity and duration of physical activity. For example, if you begin to run long distances without working your way into doing so, you will be more likely to develop a stress fracture.
Common symptoms of stress fractures are pain and swelling near the weight bearing area on the injured bone. When initial x-rays are performed, it is possible that the fracture will not show up. However, once the stress on the area continues, the damage will increase, and the fracture will be severe enough to show up on an x-ray. Certain parts of the foot are more likely to develop stress fractures than others. Areas that typically have these fractures are: the metatarsals, the navicular bone, the calcaneus, tibia, and fibula.
Since women are at an increased risk of developing osteoporosis, they are twice as likely as men to sustain a stress fracture. Additionally, old age causes a decrease in bone mineral density which is why elderly people are also likely to develop these fractures.
It is important for you to be professionally diagnosed by a podiatrist if you suspect you have a stress fracture, because there are other injuries that can easily be mistaken for a fracture. Sprains, strains, shin splints, plantar fasciitis, and Morton’s neuroma can all easily be mistaken for stress fractures in the foot. Your podiatrist will likely ask you a series of questions to determine what type of pain you are experiencing. These questions will help your doctor identify whether you have a stress fracture.
The best method of treatment for a stress fracture is rest. Additionally, a walking boot, cast, or crutches, will help rest the area that is injured. The typical healing time for stress fractures is 4-12 weeks, however this depends on which bone is involved.
The Hidden Effects of High Heels on Foot Health

Wearing high heels may enhance appearance, but they can have negative effects on foot health. High heels place added pressure on the ball of the foot, which can lead to pain, inflammation, and long-term joint stress. This unnatural positioning can also change the way a person walks, known as gait, by shortening the stride and causing instability. Over time, these changes may affect balance and coordination. High heels can also influence posture by shifting the body’s weight forward, which may disrupt the natural curves in the lower back. Limiting heel height and choosing supportive footwear more often can help protect the health and comfort of your entire body. If you enjoy wearing high heels and have developed foot pain, it is suggested that you contact a podiatrist who can offer relief solutions, and guide you on a better type of shoe to wear.
High heels have a history of causing foot and ankle problems. If you have any concerns about your feet or ankles, contact one of our podiatrists from Bangor Podiatry. Our doctors can provide the care you need to keep you pain-free and on your feet.
Effects of High Heels on the Feet
High heels are popular shoes among women because of their many styles and societal appeal. Despite this, high heels can still cause many health problems if worn too frequently.
Which Parts of My Body Will Be Affected by High Heels?
- Ankle Joints
- Achilles Tendon – May shorten and stiffen with prolonged wear
- Balls of the Feet
- Knees – Heels cause the knees to bend constantly, creating stress on them
- Back – They decrease the spine’s ability to absorb shock, which may lead to back pain. The vertebrae of the lower back may compress.
What Kinds of Foot Problems Can Develop from Wearing High Heels?
- Corns
- Calluses
- Hammertoe
- Bunions
- Morton’s Neuroma
- Plantar Fasciitis
How Can I Still Wear High Heels and Maintain Foot Health?
If you want to wear high heeled shoes, make sure that you are not wearing them every day, as this will help prevent long term physical problems. Try wearing thicker heels as opposed to stilettos to distribute weight more evenly across the feet. Always make sure you are wearing the proper shoes for the right occasion, such as sneakers for exercising. If you walk to work, try carrying your heels with you and changing into them once you arrive at work. Adding inserts to your heels can help cushion your feet and absorb shock. Full foot inserts or metatarsal pads are available.
If you have any questions please feel free to contact our offices located in Bangor, Gilbert, and Bethlehem, PA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Why High Heels Are Not Ideal for Healthy Feet
It is no secret that high heels are uncomfortable to wear for long periods of time. Although beauty is pain, you should not sacrifice the health of your feet for a stylish heel. Wearing high heels can potentially cause many different foot conditions that may be avoided by wearing proper footwear.
The structure of high heels forces weight of your body to get shifted forward toward the ball of the foot. The higher the heel you wear, the more weight and pressure get shifted forward. The pressure that your toes may experience from wearing heels may lead to hammer toes, bunions, and ingrown toenails. Extra weight and pressure resulting from wearing heels may cause stress fractures. Furthermore, heels may cause pinched nerves which may result in Morton’s neuroma.
High heels are even more dangerous for people who are clumsy. Falling or tripping while wearing heels can cause an ankle sprain or twist.
What many people don’t know is that heels can also cause back and knee problems. In order for your body to stay balanced on heels, your spine has to sway unnaturally, which adds stress to your spine muscles. This may cause you to experience a sore lower back.
If you decide to wear high heels regardless of the risks associated with them, there are ways you can minimize their harmful effects. One way to reduce injury is to massage and stretch your legs at the end of the day. Stretching can prevent the Achilles tendons and calf muscles from becoming too tight. If you are simply looking for more height, wedges and platforms provide a better surface area to distribute the body weight across compared to thinner heels.
If you experience pain from wearing high heels, it is important to see a podiatrist before any of your symptoms become worse.
Benefits of a Total Contact Cast

A total contact cast can be used to help patients with diabetic foot ulcers heal more effectively. This specialized cast, made of plaster or fiberglass, is molded to conform closely to the contours of the foot and lower leg. By distributing your weight evenly along the entire sole, the total contact cast reduces localized pressure on the ulcer site. A layer of soft foam below the ulcer further reduces pressure, helping to protect the sore and promote healing. Total contact casts are typically used when neuropathy is present, a complication of diabetes that causes reduced sensation in the feet. This loss of feeling can make it difficult to detect minor injuries, which can quickly progress into serious ulcers. By restricting unnecessary movement and limiting pressure on the ulcer, the cast supports faster healing, often within several weeks. A podiatrist monitors the progress by replacing the cast weekly and checking for complications. If you suffer from diabetic foot ulcers, it is suggested that you schedule an appointment with a podiatrist for ongoing treatment.
Diabetic foot care is important in preventing foot ailments such as ulcers. If you are suffering from diabetes or have any other concerns about your feet, contact one of our podiatrists from Bangor Podiatry. Our doctors can provide the care you need to keep you pain-free and on your feet.
Diabetic Foot Care
Diabetes affects millions of people every year. The condition can damage blood vessels in many parts of the body, especially the feet. Because of this, taking care of your feet is essential if you have diabetes, and having a podiatrist help monitor your foot health is highly recommended.
The Importance of Caring for Your Feet
- Routinely inspect your feet for bruises or sores.
- Wear socks that fit your feet comfortably.
- Wear comfortable shoes that provide adequate support.
Patients with diabetes should have their doctor monitor their blood levels, as blood sugar levels play such a huge role in diabetic care. Monitoring these levels on a regular basis is highly advised.
It is always best to inform your healthcare professional of any concerns you may have regarding your feet, especially for diabetic patients. Early treatment and routine foot examinations are keys to maintaining proper health, especially because severe complications can arise if proper treatment is not applied.
If you have any questions please feel free to contact our offices located in Bangor, Gilbert, and Bethlehem, PA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Diabetic Foot Care
Diabetes can cause two problems that can potentially affect the feet: Diabetic neuropathy and Peripheral Vascular Disease. Diabetic neuropathy occurs when nerves in your legs and feet become damaged, which prevents you from feeling heat, cold, or pain. The problem with diabetic neuropathy is that a cut or sore on the foot may go unnoticed and the cut may eventually become infected. This condition is also a main cause of foot ulcers. Additionally, Peripheral vascular disease also affects blood flow in the body. Poor blood flow will cause sores and cuts to take longer to heal. Infections that don’t heal do to poor blood flow can potentially cause ulcers or gangrene.
There are certain foot problems that are more commonly found in people with diabetes such as Athlete’s foot, calluses, corns, blisters, bunions, foot ulcers, ingrown toenails, and plantar warts. These conditions can lead to infection and serious complications such as amputation. Fortunately, proper foot care can help prevent these foot problems before they progress into more serious complications.
Each day you should wash your feet in warm water with a mild soap. When you finish washing your feet, dry them carefully especially between your toes. You should also perform daily foot inspections to ensure you don’t have any redness, blisters, or calluses. Furthermore, if you are diabetic, you should always wear closed-toed shoes or slippers to protect your feet. Practicing these tips will help ensure that your feet are kept healthy and away from infection.
If you have diabetes, contact your podiatrist if you have any of the following symptoms on your feet: changes in skin color, corns or calluses, open sores that are slow to heal, unusual and persistent odor, or changes in skin temperature. Your podiatrist will do a thorough examination of your feet to help treat these problematic conditions.
Various Causes of Foot Pain

Foot pain can affect your daily life, especially when it involves the big toe or ball of the foot. Common causes include gout, bunions, and Morton’s neuroma. Gout is a type of arthritis caused by a buildup of uric acid, often resulting in sudden, intense pain, redness, and swelling, typically in the big toe. Bunions are bony bumps that form at the base of the big toe, leading to discomfort, stiffness, and difficulty walking. Morton’s neuroma involves thickening of tissue around a nerve in the ball of the foot, causing burning pain, tingling, or numbness between the toes. These conditions can make every step feel sharp, aching, or even electric. Wearing tight shoes or standing for long periods can worsen symptoms. A podiatrist can diagnose the cause of your foot pain through a physical exam and imaging. Treatment may include custom orthotics, medication, or minor procedures to relieve pain and restore comfort. If you have ongoing foot pain, it is suggested that you schedule an appointment with a podiatrist.
Foot Pain
Foot pain can be extremely painful and debilitating. If you have a foot pain, consult with one of our podiatrists from Bangor Podiatry. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
Causes
Foot pain is a very broad condition that could be caused by one or more ailments. The most common include:
- Bunions
- Hammertoes
- Plantar Fasciitis
- Bone Spurs
- Corns
- Tarsal Tunnel Syndrome
- Ingrown Toenails
- Arthritis (such as Gout, Rheumatoid, and Osteoarthritis)
- Flat Feet
- Injury (from stress fractures, broken toe, foot, ankle, Achilles tendon ruptures, and sprains)
- And more
Diagnosis
To figure out the cause of foot pain, podiatrists utilize several different methods. This can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatment depends upon the cause of the foot pain. Whether it is resting, staying off the foot, or having surgery; podiatrists have a number of treatment options available for foot pain.
If you have any questions, please feel free to contact our offices located in Bangor, Gilbert, and Bethlehem, PA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Blog Archives
- July 2025
- June 2025
- May 2025
- April 2025
- March 2025
- February 2025
- January 2025
- December 2024
- November 2024
- October 2024
- September 2024
- August 2024
- July 2024
- June 2024
- May 2024
- April 2024
- March 2024
- February 2024
- January 2024
- December 2023
- November 2023
- October 2023
- September 2023
- August 2023
- July 2023
- June 2023
- May 2023
- April 2023
- March 2023
- February 2023
- January 2023