Connect With Us

The Hidden Effects of High Heels on Foot Health

Wearing high heels may enhance appearance, but they can have negative effects on foot health. High heels place added pressure on the ball of the foot, which can lead to pain, inflammation, and long-term joint stress. This unnatural positioning can also change the way a person walks, known as gait, by shortening the stride and causing instability. Over time, these changes may affect balance and coordination. High heels can also influence posture by shifting the body’s weight forward, which may disrupt the natural curves in the lower back. Limiting heel height and choosing supportive footwear more often can help protect the health and comfort of your entire body. If you enjoy wearing high heels and have developed foot pain, it is suggested that you contact a podiatrist who can offer relief solutions, and guide you on a better type of shoe to wear.
High heels have a history of causing foot and ankle problems. If you have any concerns about your feet or ankles, contact one of our podiatrists from Bangor Podiatry. Our doctors can provide the care you need to keep you pain-free and on your feet.
Effects of High Heels on the Feet
High heels are popular shoes among women because of their many styles and societal appeal. Despite this, high heels can still cause many health problems if worn too frequently.
Which Parts of My Body Will Be Affected by High Heels?
- Ankle Joints
- Achilles Tendon – May shorten and stiffen with prolonged wear
- Balls of the Feet
- Knees – Heels cause the knees to bend constantly, creating stress on them
- Back – They decrease the spine’s ability to absorb shock, which may lead to back pain. The vertebrae of the lower back may compress.
What Kinds of Foot Problems Can Develop from Wearing High Heels?
- Corns
- Calluses
- Hammertoe
- Bunions
- Morton’s Neuroma
- Plantar Fasciitis
How Can I Still Wear High Heels and Maintain Foot Health?
If you want to wear high heeled shoes, make sure that you are not wearing them every day, as this will help prevent long term physical problems. Try wearing thicker heels as opposed to stilettos to distribute weight more evenly across the feet. Always make sure you are wearing the proper shoes for the right occasion, such as sneakers for exercising. If you walk to work, try carrying your heels with you and changing into them once you arrive at work. Adding inserts to your heels can help cushion your feet and absorb shock. Full foot inserts or metatarsal pads are available.
If you have any questions please feel free to contact our offices located in Bangor, Gilbert, and Bethlehem, PA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Why High Heels Are Not Ideal for Healthy Feet
It is no secret that high heels are uncomfortable to wear for long periods of time. Although beauty is pain, you should not sacrifice the health of your feet for a stylish heel. Wearing high heels can potentially cause many different foot conditions that may be avoided by wearing proper footwear.
The structure of high heels forces weight of your body to get shifted forward toward the ball of the foot. The higher the heel you wear, the more weight and pressure get shifted forward. The pressure that your toes may experience from wearing heels may lead to hammer toes, bunions, and ingrown toenails. Extra weight and pressure resulting from wearing heels may cause stress fractures. Furthermore, heels may cause pinched nerves which may result in Morton’s neuroma.
High heels are even more dangerous for people who are clumsy. Falling or tripping while wearing heels can cause an ankle sprain or twist.
What many people don’t know is that heels can also cause back and knee problems. In order for your body to stay balanced on heels, your spine has to sway unnaturally, which adds stress to your spine muscles. This may cause you to experience a sore lower back.
If you decide to wear high heels regardless of the risks associated with them, there are ways you can minimize their harmful effects. One way to reduce injury is to massage and stretch your legs at the end of the day. Stretching can prevent the Achilles tendons and calf muscles from becoming too tight. If you are simply looking for more height, wedges and platforms provide a better surface area to distribute the body weight across compared to thinner heels.
If you experience pain from wearing high heels, it is important to see a podiatrist before any of your symptoms become worse.
Benefits of a Total Contact Cast

A total contact cast can be used to help patients with diabetic foot ulcers heal more effectively. This specialized cast, made of plaster or fiberglass, is molded to conform closely to the contours of the foot and lower leg. By distributing your weight evenly along the entire sole, the total contact cast reduces localized pressure on the ulcer site. A layer of soft foam below the ulcer further reduces pressure, helping to protect the sore and promote healing. Total contact casts are typically used when neuropathy is present, a complication of diabetes that causes reduced sensation in the feet. This loss of feeling can make it difficult to detect minor injuries, which can quickly progress into serious ulcers. By restricting unnecessary movement and limiting pressure on the ulcer, the cast supports faster healing, often within several weeks. A podiatrist monitors the progress by replacing the cast weekly and checking for complications. If you suffer from diabetic foot ulcers, it is suggested that you schedule an appointment with a podiatrist for ongoing treatment.
Diabetic foot care is important in preventing foot ailments such as ulcers. If you are suffering from diabetes or have any other concerns about your feet, contact one of our podiatrists from Bangor Podiatry. Our doctors can provide the care you need to keep you pain-free and on your feet.
Diabetic Foot Care
Diabetes affects millions of people every year. The condition can damage blood vessels in many parts of the body, especially the feet. Because of this, taking care of your feet is essential if you have diabetes, and having a podiatrist help monitor your foot health is highly recommended.
The Importance of Caring for Your Feet
- Routinely inspect your feet for bruises or sores.
- Wear socks that fit your feet comfortably.
- Wear comfortable shoes that provide adequate support.
Patients with diabetes should have their doctor monitor their blood levels, as blood sugar levels play such a huge role in diabetic care. Monitoring these levels on a regular basis is highly advised.
It is always best to inform your healthcare professional of any concerns you may have regarding your feet, especially for diabetic patients. Early treatment and routine foot examinations are keys to maintaining proper health, especially because severe complications can arise if proper treatment is not applied.
If you have any questions please feel free to contact our offices located in Bangor, Gilbert, and Bethlehem, PA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Diabetic Foot Care
Diabetes can cause two problems that can potentially affect the feet: Diabetic neuropathy and Peripheral Vascular Disease. Diabetic neuropathy occurs when nerves in your legs and feet become damaged, which prevents you from feeling heat, cold, or pain. The problem with diabetic neuropathy is that a cut or sore on the foot may go unnoticed and the cut may eventually become infected. This condition is also a main cause of foot ulcers. Additionally, Peripheral vascular disease also affects blood flow in the body. Poor blood flow will cause sores and cuts to take longer to heal. Infections that don’t heal do to poor blood flow can potentially cause ulcers or gangrene.
There are certain foot problems that are more commonly found in people with diabetes such as Athlete’s foot, calluses, corns, blisters, bunions, foot ulcers, ingrown toenails, and plantar warts. These conditions can lead to infection and serious complications such as amputation. Fortunately, proper foot care can help prevent these foot problems before they progress into more serious complications.
Each day you should wash your feet in warm water with a mild soap. When you finish washing your feet, dry them carefully especially between your toes. You should also perform daily foot inspections to ensure you don’t have any redness, blisters, or calluses. Furthermore, if you are diabetic, you should always wear closed-toed shoes or slippers to protect your feet. Practicing these tips will help ensure that your feet are kept healthy and away from infection.
If you have diabetes, contact your podiatrist if you have any of the following symptoms on your feet: changes in skin color, corns or calluses, open sores that are slow to heal, unusual and persistent odor, or changes in skin temperature. Your podiatrist will do a thorough examination of your feet to help treat these problematic conditions.
Various Causes of Foot Pain

Foot pain can affect your daily life, especially when it involves the big toe or ball of the foot. Common causes include gout, bunions, and Morton’s neuroma. Gout is a type of arthritis caused by a buildup of uric acid, often resulting in sudden, intense pain, redness, and swelling, typically in the big toe. Bunions are bony bumps that form at the base of the big toe, leading to discomfort, stiffness, and difficulty walking. Morton’s neuroma involves thickening of tissue around a nerve in the ball of the foot, causing burning pain, tingling, or numbness between the toes. These conditions can make every step feel sharp, aching, or even electric. Wearing tight shoes or standing for long periods can worsen symptoms. A podiatrist can diagnose the cause of your foot pain through a physical exam and imaging. Treatment may include custom orthotics, medication, or minor procedures to relieve pain and restore comfort. If you have ongoing foot pain, it is suggested that you schedule an appointment with a podiatrist.
Foot Pain
Foot pain can be extremely painful and debilitating. If you have a foot pain, consult with one of our podiatrists from Bangor Podiatry. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
Causes
Foot pain is a very broad condition that could be caused by one or more ailments. The most common include:
- Bunions
- Hammertoes
- Plantar Fasciitis
- Bone Spurs
- Corns
- Tarsal Tunnel Syndrome
- Ingrown Toenails
- Arthritis (such as Gout, Rheumatoid, and Osteoarthritis)
- Flat Feet
- Injury (from stress fractures, broken toe, foot, ankle, Achilles tendon ruptures, and sprains)
- And more
Diagnosis
To figure out the cause of foot pain, podiatrists utilize several different methods. This can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatment depends upon the cause of the foot pain. Whether it is resting, staying off the foot, or having surgery; podiatrists have a number of treatment options available for foot pain.
If you have any questions, please feel free to contact our offices located in Bangor, Gilbert, and Bethlehem, PA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Foot Pain
Our feet are arguably the most important parts of our bodies because they are responsible for getting us from place to place. However, we often don’t think about our feet until they begin to hurt. If you have pain in your feet, you need to first determine where on the foot you are experiencing it to get to the root of the problem. The most common areas to feel pain on the foot are the heel and the ankle.
Heel pain is most commonly attributed to a condition called plantar fasciitis. Plantar fasciitis occurs when the plantar fascia, which is the band of tough tissue connecting the heel bone to the toes becomes inflamed. Plantar fasciitis pain is usually worse in the morning, and it tends to go away throughout the day. If you have plantar fasciitis, you should rest your foot and do heel and foot muscles stretches. Wearing shoes with proper arch support and a cushioned sole has also been proven to be beneficial.
Some common symptoms of foot pain are redness, swelling, and stiffness. Foot pain can be dull or sharp depending on its underlying cause. Toe pain can also occur, and it is usually caused by gout, bunions, hammertoes, ingrown toenails, sprains, fractures, and corns.
If you have severe pain in your feet, you should immediately seek assistance from your podiatrist for treatment. Depending on the cause of your pain, your podiatrist may give you a variety of treatment options.
Relieving Heel Pain From Plantar Fasciitis

Plantar fasciitis is one of the most common causes of heel pain, often felt as a sharp or stabbing sensation with the first steps in the morning or after rest. It results from inflammation of the plantar fascia, the thick band of tissue that supports the arch and connects the heel to the toes. Diagnosis begins with a podiatrist reviewing your symptoms and medical history, followed by a physical exam to check for tenderness and tightness along the bottom of the foot. Imaging such as X-rays may be used to rule out other causes. Treatment typically includes rest, stretching exercises, wearing supportive footwear, or custom orthotics. In more persistent cases, targeted exercises, night splints, or anti-inflammatory treatments may be recommended. Addressing plantar fasciitis early helps prevent chronic pain or altered walking patterns. If heel pain is interfering with your daily life, it is suggested that you see a podiatrist.
Plantar fasciitis can be very painful and inconvenient. If you are experiencing heel pain or symptoms of plantar fasciitis, contact one of our podiatrists from Bangor Podiatry. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the thick band of tissue that runs along the bottom of your foot, known as the plantar fascia, and causes mild to severe heel pain.
What Causes Plantar Fasciitis?
- Excessive running
- Non-supportive shoes
- Overpronation
- Repeated stretching and tearing of the plantar fascia
How Can It Be Treated?
- Conservative measures – anti-inflammatories, ice packs, stretching exercises, physical therapy, orthotic devices
- Shockwave therapy – sound waves are sent to the affected area to facilitate healing and are usually used for chronic cases of plantar fasciitis
- Surgery – usually only used as a last resort when all else fails. The plantar fascia can be surgically detached from the heel
While very treatable, plantar fasciitis is definitely not something that should be ignored. Especially in severe cases, speaking to your doctor right away is highly recommended to avoid complications and severe heel pain. Your podiatrist can work with you to provide the appropriate treatment options tailored to your condition.
If you have any questions please feel free to contact our offices located in Bangor, Gilbert, and Bethlehem, PA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Plantar Fasciitis
The plantar fascia is a connective tissue in the heel that stretches across the bottom length of your foot. Plantar fasciitis occurs when the connective tissue becomes inflamed, causing heel pain and discomfort during physical activity. Although the condition is completely treatable, traditional methods can take up to a year to start becoming effective.
Plantar fasciitis is caused by a number of everyday activities, so understanding the condition is important for managing and treating it. One of the most common causes of plantar fasciitis is excessive running, especially with improper fitting or non-supportive shoes. Too much exercise can lead to the plantar fascia being overworked and overstretched, which can cause tears in the tissue. Along with improper fitting shoes, pronation, the rolling of the feet inward, is a common cause of plantar fasciitis. If not treated properly, the plantar fascia becomes overstretched and starts to tear, causing inflammation.
Despite the common causes of plantar fasciitis, there are many different treatment options. For less severe cases, conservative home remedies include taking anti-inflammatory drugs to alleviate pain, applying ice packs to the bottom of your foot and heel, slowly stretching and exercising your feet to re-strengthen the tissue, and using orthotic devices are all ways to help manage your plantar fasciitis.
For more severe cases, shockwave therapy has become a common solution for plantar fasciitis. Shockwave therapy can effectively break up the tissue on the bottom of your foot which facilitates healing and regeneration. This fights the chronic pain caused by plantar fasciitis. Even if this doesn’t work, surgery is always a final option. Surgery on the tissue itself can be done to permanently correct the issue and stop the inflammation and pain in your heels.
No matter what the case may be, consulting your podiatrist is the first and best step to recovery. Even the slightest amount of heel pain could be the first stage of plantar fasciitis. Untreated symptoms can lead to the tearing and overstretching of tissue. Because the tearing of tissue can be compounded if it remains ignored, it can evolve into a severe case. The solution is early detection and early treatment. Talk to your podiatrist about the possibilities of plantar fasciitis if you’re experiencing heel pain.
Noticing the First Signs of Arthritis in Your Feet
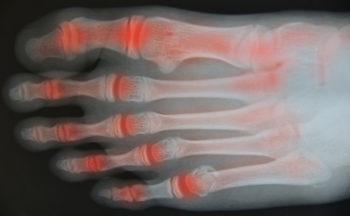
Arthritis often starts subtly, especially in the feet and ankles, where the early signs can be mistaken for general wear and tear. You may feel stiffness in the morning that eases as the day goes on, or notice swelling that becomes more frequent after activity. Some people experience aching in the joints or difficulty walking longer distances without discomfort. Pain may seem to come and go, making it easy to ignore until it worsens. Over time, joint mobility may decrease, shoes may feel tighter, or you may even hear a grinding sound when moving. These early signs should not be dismissed, as timely intervention can slow progression and help preserve joint function. Arthritis in the feet can affect your balance, mobility, and overall comfort, impacting your quality of life. If you are noticing any of these changes, it is suggested that you see a podiatrist for effective relief and treatment solutions.
Arthritis can be a difficult condition to live with. If you are seeking treatment, contact one of our podiatrists from Bangor Podiatry. Our doctors can provide the care you need to keep you pain-free and on your feet.
Arthritic Foot Care
Arthritis is a term that is commonly used to describe joint pain. The condition itself can occur to anyone of any age, race, or gender, and there are over 100 types of it. Nevertheless, arthritis is more commonly found in women compared to men, and it is also more prevalent in those who are overweight. The causes of arthritis vary depending on which type of arthritis you have. Osteoarthritis for example, is often caused by injury, while rheumatoid arthritis is caused by a misdirected immune system.
Symptoms
- Swelling
- Pain
- Stiffness
- Decreased Range of Motion
Arthritic symptoms range in severity, and they may come and go. Some symptoms stay the same for several years but could potentially get worse with time. Severe cases of arthritis can prevent its sufferers from performing daily activities and make walking difficult.
Risk Factors
- Occupation – Occupations requiring repetitive knee movements have been linked to osteoarthritis
- Obesity – Excess weight can contribute to osteoarthritis development
- Infection – Microbial agents can infect the joints and trigger arthritis
- Joint Injuries – Damage to joints may lead to osteoarthritis
- Age – Risk increases with age
- Gender –Most types are more common in women
- Genetics – Arthritis can be hereditary
If you suspect your arthritis is affecting your feet, it is crucial that you see a podiatrist immediately. Your doctor will be able to address your specific case and help you decide which treatment method is best for you.
If you have any questions, please feel free to contact our offices located in Bangor, Gilbert, and Bethlehem, PA . We offer the newest diagnostic and treatment technologies for all your foot care needs.